New York State issued a notice to plans and PBMs stating that each plan must implement point of sale (POS) claim denial messaging that directs pharmacies to bill NYRx for Medicaid Pharmacy Program effective April 1, 2023. The state provided PBMs with specific instructions on the NCPDP reject code and message that they expected to return on these members' claims. Other PBMs lobbied to eliminate this POS requirement, saying it was "not possible" to implement within the allowed time frame.
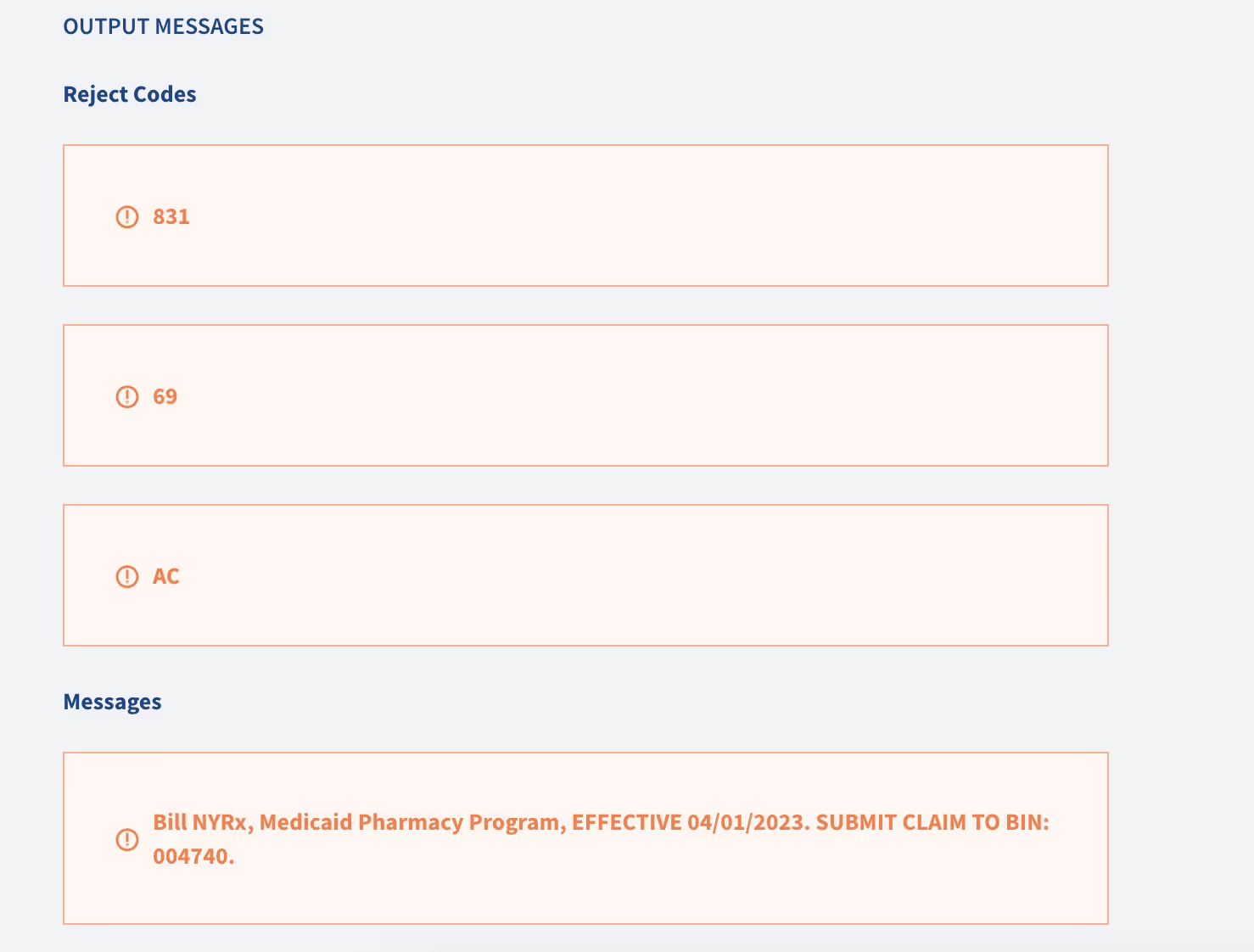
With Judi's Tag and Override features, we were able to configure the NCPDP reject code and message requirement in less time than the meeting took. We created a tag that targeted claims that were going to reject for NCPDP code 69, as these members' coverage was set to terminate on March 31, 2023. We then defined the expected actions via an override, adding a reject (831) and message exactly as directed by the state. After applying the override to claims within the supplied date range, we tested a claim before and after applying the override.
The outcome? Claims were paid as our client intended for dates of service before the newly implemented override and rejected with the NCPDP 831 code plus POS messaging provided by NYS for dates of service starting 4/1/2023.
Ju's flexibility and adaptability allowed us to implement the POS claim denial messaging for our clients, ensuring compliance with state requirements while minimizing any disruption